PEMBERDAYAAN KADER TANGGUH PEDULI LEPRA DALAM PELACAKAN KUSTA
EMPOWERMENT OF TANGGUH CARE FOR LEPRA IN LEPROSY TRACKING
DOI:
https://doi.org/10.36341/jpm.v7i1.3824Keywords:
Empowerment of cadres, knowledge, early detection of leprosyAbstract
Introduction: Social problems caused by leprosy arise due to the fear that leprosy sufferers experience in society (leprophobia). Low knowledge, lack of socialization in society, and bad stigma in society, resulting in a lack of community participation in eradicating leprosy. After India and Brazil, Indonesia is one of the developing countries with the highest number of newly diagnosed sufferers. leprosy case. third highest in the world. Purpose: The purpose of this community service is to increase public understanding of early detection of leprosy in Kolo Kota Bima Village. Method: The method used in this community service is health education and training on the identification of leprosy by tough cadres caring for leprosy. Community service activities were carried out in the Kolo Community Health Center hall, Bima City, which was attended by 15 cadres, 5 enumerators, the Head of the Kolo Community Health Center, the KTU of the Kolo Health Center, and servants. This activity is training for cadres and counseling about leprosy including the meaning, signs, symptoms, management, process of transmission of leprosy. Results: The results of the pre-test community service were 27% of cadres with good knowledge. While the post test 100% of cadres have good knowledge. The results of this dedication are important to assist the government's efforts to improve national health development. Conclusions and Recommendations: All targeted leprosy care cadres have understood the signs and symptoms of leprosy. It is hoped that community service will be carried out regularly and to health cadres so that leprosy cases can be handled immediately.
Downloads
References
L. C. Rodrigues and D. N. J. Lockwood, “Leprosy now: Epidemiology, progress, challenges, and research gaps,†Lancet Infect. Dis., vol. 11, no. 6, pp. 464–470, 2011, doi: 10.1016/S1473-3099(11)70006-8.
R. Singh, B. Singh, and S. Mahato, “Community knowledge, attitude, and perceived stigma of leprosy amongst community members living in Dhanusha and Parsa districts of Southern Central Nepal,†PLoS Negl. Trop. Dis., vol. 13, no. 1, pp. 1–19, 2019, doi: 10.1371/journal.pntd.0007075.
C. S. Smith et al., “A strategy to halt leprosy transmission,†Lancet Infect. Dis., vol. 14, no. 2, pp. 96–98, 2014, doi: 10.1016/S1473-3099(13)70365-7.
D. N. J. Lockwood, V. Shetty, and G. Oliveira, “Hazards of setting targets to eliminate disease: Lessons from the leprosy elimination campaign,†BMJ, vol. 348, no. February, pp. 3–8, 2014, doi: 10.1136/bmj.g1136.
World Health Organization (WHO), Global Leprosy Strategy 2016–2020. New Delhi india: World Health Organization, Regional Office for South-East Asia., 2020.
M. I. Bakker et al., “Population survey to determine risk factors for Mycobacterium leprae transmission and infection,†Int. J. Epidemiol., vol. 33, no. 6, pp. 1329–1336, 2004, doi: 10.1093/ije/dyh266.
V. Martinez Dominguez et al., “Epidemiological information on leprosy in the Singu area of Upper Burma,†Bull. World Health Organ., vol. 58, no. 1, pp. 81–89, 1980.
J. a Doull, “The incidence of leprosy in Cordova and Talisay, Cebu, Philippines,†Int J Lepr, vol. 10, pp. 107–131, 1942.
S. Ramasamy, A. Kumar, and P. Govindharaj, “Screening household contacts of children diagnosed with leprosy in a tertiary referral centre, Chhattisgarh State, India,†Lepr. Rev., vol. 89, no. 2, pp. 117–123, 2018, doi: 10.47276/lr.89.2.117.
A. M. Sales et al., “Leprosy among patient contacts: A multilevel study of risk factors,†PLoS Negl. Trop. Dis., vol. 5, no. 3, pp. 1–6, 2011, doi: 10.1371/journal.pntd.0001013.
J. M. Pescarini et al., “Socioeconomic risk markers of leprosy in high-burden countries: A systematic review and meta-analysis,†PLoS Negl. Trop. Dis., vol. 12, no. 7, pp. 1–20, 2018, doi: 10.1371/journal.pntd.0006622.
D. A. Haake and P. N. Levett, “Leptospirosis in Humans,†J. Biol. Educ., vol. 387, no. may, pp. 65–97, 2015, doi: 10.1080/00219266.1991.9655201.
F. Costa et al., “Global Morbidity and Mortality of Leptospirosis: A Systematic Review,†PLoS Negl. Trop. Dis., vol. 9, no. 9, pp. 0–1, 2015, doi: 10.1371/journal.pntd.0003898.
P. R. Torgerson et al., “Global Burden of Leptospirosis: Estimated in Terms of Disability Adjusted Life Years,†PLoS Negl. Trop. Dis., vol. 9, no. 10, pp. 1–14, 2015, doi: 10.1371/journal.pntd.0004122.
C. L. Lau, L. D. Smythe, S. B. Craig, and P. Weinstein, “Climate change, flooding, urbanisation and leptospirosis: Fuelling the fire?,†Trans. R. Soc. Trop. Med. Hyg., vol. 104, no. 10, pp. 631–638, 2010, doi: 10.1016/j.trstmh.2010.07.002.
M. C. Schneider et al., “Leptospirosis in Latin America: exploring the first set of regional data Original research,†Pan Am. J. Public Heal., vol. 41, pp. 1–9, 2017, [Online]. Available: http://www.healthmap.org/en/
F. Costa, M. S. Martinez-Silveira, J. E. Hagan, R. A. Hartskeerl, M. G. Dos Reis, and A. I. Ko, “Surveillance for leptospirosis in the Americas, 1996-2005: A review of data from ministries of health,†Rev. Panam. Salud Publica/Pan Am. J. Public Heal., vol. 32, no. 3, pp. 169–177, 2012, doi: 10.1590/S1020-49892012000900001.
L. school of hygiene & tropical Medicine, Leprosy and the eye teaching set. 2010.
E. Haverkort and A. T. van ‘t Noordende, “Health workers’ perceptions of leprosy and factors influencing their perceptions in endemic countries: A systematic literature review,†Lepr. Rev., vol. 93, no. 4, pp. 332–347, 2022, doi: 10.47276/lr.93.4.332.
E. Broadbent, C. Wilkes, H. Koschwanez, J. Weinman, S. Norton, and K. J. Petrie, “A systematic review and meta-analysis of the Brief Illness Perception Questionnaire,†Psychol. Heal., vol. 30, no. 11, pp. 1361–1385, 2015, doi: 10.1080/08870446.2015.1070851.
F. A. Rincón Uribe et al., “Health knowledge, health behaviors and attitudes during pandemic emergencies: A systematic review,†PLoS One, vol. 16, no. 9, p. e0256731, 2021, doi: 10.1371/journal.pone.0256731.
Z. He et al., “Factors influencing health knowledge and behaviors among the elderly in rural China,†Int. J. Environ. Res. Public Health, vol. 13, no. 10, pp. 1–16, 2016, doi: 10.3390/ijerph13100975.
C. T. Garma, “Psychosocial Intervention review,†Psychosoc. Interv., vol. 26, no. 2, pp. 73–91, 2017, [Online]. Available: http://dx.doi.org/10.1016/j.psi.2016.11.001
V. Raghupathi and W. Raghupathi, “The influence of education on health: An empirical assessment of OECD countries for the period 1995-2015,†Arch. Public Heal., vol. 78, no. 1, pp. 1–18, 2020, doi: 10.1186/s13690-020-00402-5.
J. Mirowsky and C. E. Ross, Education, Social Status And Health. New York: Routledge, 2017.
C. E. A. Higgins, Health Impacts of Education a review. 2008.
Tesema AA and Beriso M, “Assessment of Knowledge and Attitude of Community on Leprosy Patients in Kuyera Town, West Arsi Zone, Oromia Region Southeast Ethiopia,†Hered. Genet., vol. 05, no. 01, pp. 1–6, 2016, doi: 10.4172/2161-1041.1000156.
D. R. Bajaj, B. L. Matlani, F. R. Soomro, and M. P. Iqbal, “Knowledge, altitude and practices regarding leprosy among general practitioners at Hyderabad,†J. Coll. Physicians Surg. Pakistan, vol. 19, no. 4, pp. 215–218, 2009.
R. Tooher, J. E. Collins, J. M. Street, A. Braunack-Mayer, and H. Marshall, “Community knowledge, behaviours and attitudes about the 2009 H1N1 Influenza pandemic: A systematic review,†Influenza Other Respi. Viruses, vol. 7, no. 6, pp. 1316–1327, 2013, doi: 10.1111/irv.12103.
H. H. Balkhy, M. A. Abolfotouh, R. H. Al-Hathlool, and M. A. Al-Jumah, “Awareness, attitudes, and practices related to the swine influenza pandemic among the Saudi public,†BMC Infect. Dis., vol. 10, no. 42, pp. 1–7, 2010, doi: 10.1186/1471-2334-10-42.
G. Di Giuseppe, R. Abbate, L. Albano, P. Marinelli, and I. F. Angelillo, “A survey of knowledge, attitudes and practices towards avian influenza in an adult population of Italy,†BMC Infect. Dis., vol. 8, no. March, pp. 1–8, 2008, doi: 10.1186/1471-2334-8-36.
I. F. Angelillo, N. M. A. Viggiani, L. Rizzo, and A. Bianco, “Food handlers and foodborne diseases: Knowledge, attitudes, and reported behavior in Italy,†J. Food Prot., vol. 63, no. 3, pp. 381–385, 2000, doi: 10.4315/0362-028X-63.3.381.
Downloads
Published
How to Cite
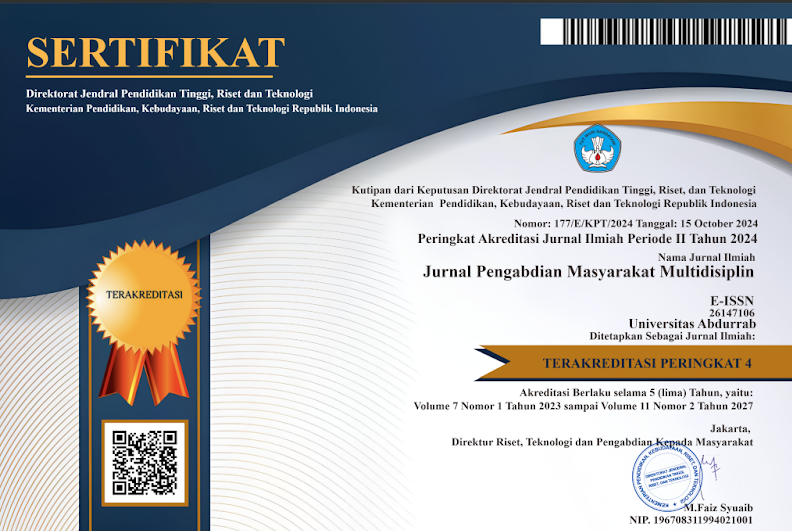
Issue
Section
License
1. Copyright of all journal manuscripts is held by the Jurnal Pengabdian Masyarakat Multidisiplin.Formal legal provisions to access digital articles of electronic journal are subject to the provision of the Creative
2. Commons Attribution-ShareAlike license (CC BY-NC-SA), which means that Jurnal Pengabdian Masyarakat Multidisiplin is rightful to keep, transfer media/format, manage in the form of databases, maintain, and
3. publish articles.Published manuscripts both printed and electronic are open access for educational, research, and library purposes. Additionally, the editorial board is not responsible for any violations of copyright law.
licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.