The Relationship Between the Use of Combination Antidiabetic and Antihipertensive Drug of Classes on the Incidence of Drug Interaction in BPJS Patients
Abstract
Diabetes mellitus and hypertension are chronic diseases that require long-term therapy, patients will receive a combination of more than two types of drugs. Therapy with two or more types of drugs can cause drug interactions that have an impact on the patient's treatment. Chronic complications can affect body organs, including morbidity and mortality. The aim of this study was to determine the incidence of drug interactions when using a combination of antidiabetic and antihypertensive drug classes and to determine the relationship between the use of a combination of antidiabetic and antihypertensive drug classes on the incidence of drug interactions. This research was conducted prospectively on drug prescriptions for type 2 diabetes mellitus patients with hypertension in BPJS referral patients at Waras Purwodadi Pharmacy. A total of 51 samples were obtained. Data were analyzed descriptively to see the incidence of drug interactions using Stockley's Drug Interactions Eight Edition 2008, Drug Interaction Facts 2009, Medscape Drug Interaction Checker Application, and Drug Interaction Checker (Drugs.com). Data analysis was analyzed using SPSS using the Chi-Square test. There were drug interactions in 44 prescriptions (86.3%) and there were no drug interactions in 7 prescriptions (13.7%). The results of the Chi-Square test showed that there was a relationship between the use of combination of antidiabetic and antihypertensive drug of classes on the incidence of drug interactions in BPJS patients, with a value of P = 0.000 (P < 0.05). The conclusion is that there is a significant relationship Between The Use of Combination Antidiabetic and Antihipertensive drug of Classes On The Incidence Of Drug Interaction In BPJS Patients
References
DinKes JawaTengah. 2018. Profil Kesehatan Provinsi Jawa Tengah Tahun 2018. Semarang: Dinas Kesehatan Provinsi Jawa Tengah. 95-98.
Hidayati, N. R., Oktaviani, P., dan Setyaningsih, I. 2018. Gambaran Interaksi Obat Diabetes Melitus Tipe 2 Dengan Obat Penyakit Penyerta Pada Pasien Rawat Inap Di Rsud Gunung Jati Kota Cirebon Tahun 2016. Jurnal Medical Sains, 2(2), 58–64.
Hestina, D. W. 2017. Faktor-Faktor Yang Berhubungan Dengan Kepatuhan Dalam Pengelolaan Diet Pada Pasien Rawat Jalan Diabetes Mellitus Tipe 2 di Kota Semarang. Journal Of Health Education, 2(2), 137–145.
International Diabetes Federation. 2015. IDF Diabetes Atlas 7th Edition. UK: International Diabetes Federation.
James, P. A., Oparil, S., Carter, B. L., Cushman, W. C., Dennison-Himmelfarb, C., Handler, J., Lackland, D. T., Lefevre, M. L., Mackenzie, T. D., Ogedegbe, O., Smith, S. C., Svetkey, L. P., Taler, S. J., Townsend, R., Wright, J. T., Narva, A. S., and Ortiz, E. 2014. Evidence-Based Guideline For The Management Of High Blood Pressure In Adults Report From The Panel Members Appointed To The Eighth Joint National Committee (JNC 8). JAMA-Journal of thr American Medical Association. 311(5), 507–520.
Jameson, J. L. 2010. Harrison’s Endocrinology Second Edition. The Mcgraw-Hill Companies: United states of America267-313.
JNC-8. 2014. The Eight Report of the Joint National Commite. Hypertension Guidelines: An In-Depth Guide. American J Manag Care.
Kashyap, M., D’Cruz, S., Sachdev, A., and Tiwari P. 2013. Drug-Drug Interactions And Their Predictors: Results From Indian Elderly Inpatients. Pharm Pract (Granada). 11(4): 191–195
Njoto, E. N. 2014. Target Tekanan Darah Pada Diabetes Melitus. Cermin Dunia Kedokteran. 41(11), 864–866.
Pasaribu, E. 2018. Analisis Interaksi Pada Pengobatan Diabetes Mellitus Tipe 2 Pasien Geriatri Di Instalasi Rawat Inap Rumah Sakit Umum Pusat (RSUP) Dr. Soeradji Tirtonegoro Tahun 2017. Skripsi. Solo: Fakultas Farmasi Universitas Setia Budi Surakarta.
Perkeni. 2015. Konsensus: Pengelolaan Dan Pencegahan Diabetes Melitus Tipe 2 di Indonesia 2015. Jakarta: Perkumpulan Endokrinologi Indonesia.
Rahmawaty, A dan Hidayah, P. H. 2020. Hubungan Drug Related Problems (DRPs) Kategori Interaksi Obat pada Penggunaan Obat Pasien Diabetes Mellitus Tipe 2. Cendekia Journal Of Pharmacy, 4(1):80-88
Rahmawaty, A dan Pratiwi, Y. 2022. Kejadian Drug Related Problems (DRPS) Interaksi Obat Dalam Peresepan Polifarmasi Pada Pasien Prolanis di Fasilitas Kesehatan Dasar Dokter X Kabupaten Kudus, Cendekia Journal Of Pharmacy, 6(1):1-13
Reinhard, E., Kamaluddin, M. T., dan Melizah, A. 2019. Potensi Terjadinya Interaksi Obat Antidiabetik Oral Pada Pasien Diabetes Melitus Tipe 2 Usia Lanjut. Sriwijaya Journal Of Medicine, 2(3), 205–210.
RISKESDAS. 2019. Laporan Hasil Riset Kesehatan Dasar (RISKESDAS) Indonesia tahun 2018. Jakarta: Badan Penelitian dan Pengembangan Kesehatan.
Sari, I. N. 2015. Evaluasi Drug Related Problems Obat Antidiabetes Pada Pasien Geriatri Dengan Diabetes Melitus Tipe 2 Di Ruang Rawat Inap RSU Pelabuhan Periode Januari-Juni 2014. Skripsi. Jakarta: Fakultas Kedokteran dan Ilmu Kesehatan, Universitas Islam negeri Syarif Hidayatullah.
Septiyana, R., Padmanegara, H. S., dan Larasati, S. 2015. Evaluasi Kerasionalan Peresepan Obat Anti Diabetes Militus Oral Pada Pasien Prolanis BPJS Di Rumah Sakit Islam Kendal. Jurnal Farmasetis, 4(1), 11–16.
Trisnawati, S. K., dan Setyorogo, S. 2013. Faktor Risiko Kejadian Diabetes Melitus Tipe 2 Di Puskesmas Kecamatan Cengkareng Jakarta Barat Tahun 2012. Jurnal Ilmiah Kesehatan, 5(1), 6–11.
Wells, B. G., Dipiro, J. T., Schwinghammer, T. L., & Dipiro, C. V. 2015. Pharmacotherapy Handbook Ninth Edition. USA: In Mcgraw-Hill Education.
World Health Organization (WHO). 2016. Global Report On Diabetes. Geneva Switzerland : WHO Press.
Yu S, Guo X, Yang H, Zheng L and Sun X. 2014. An Update On The Prevalence Of Metabolic Syndrome And Its Associated Factors In Rural Northeast China. Biomed Central Public Health, 14:877.
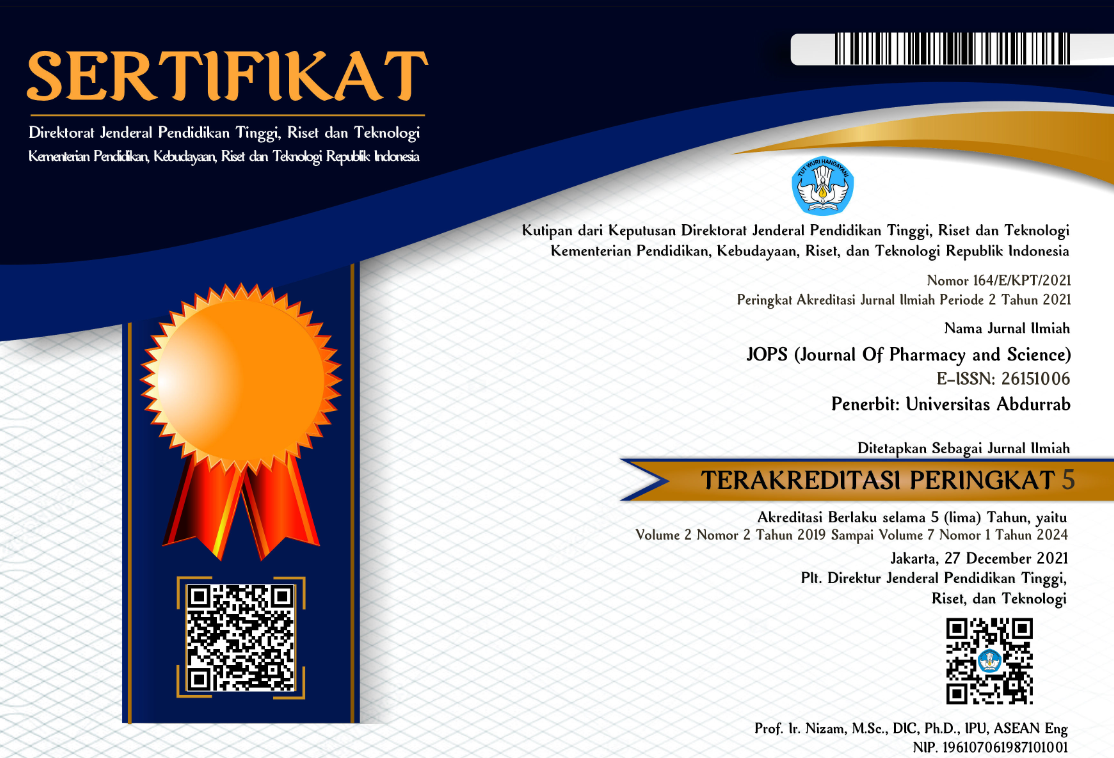
Copyright (c) 2023 JOPS (Journal Of Pharmacy and Science)

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
1. Copyright of all journal manuscripts is held by the JOPS (Journal Of Pharmacy and Science)
2. Formal legal provisions to access digital articles of electronic journal are subject to the provision of the Creative Commons Attribution-ShareAlike license (CC BY-NC-SA), which means that JOPS (Journal Of Pharmacy and Science) is rightful to keep, transfer media/format, manage in the form of databases, maintain, and publish articles.
3. Published manuscripts both printed and electronic are open access for educational, research, and library purposes. Additiponally, the editorial board is not responsible for any violations of copyright law.
licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
 PDF (Bahasa Indonesia)
PDF (Bahasa Indonesia)
 Abstract views: 109
Abstract views: 109
 downloads: 105
downloads: 105

 :
:
1.png)